In the fast-paced environment of urgent care centers, accurate coding is essential to ensure proper billing and avoid costly mistakes. Errors in medical coding can lead to denied claims, reduced reimbursements, and compliance issues. As an Urgent Care Medical Billing Expert Miami, FL, understanding common coding errors and how to avoid them can significantly enhance the efficiency and profitability of urgent care facilities.
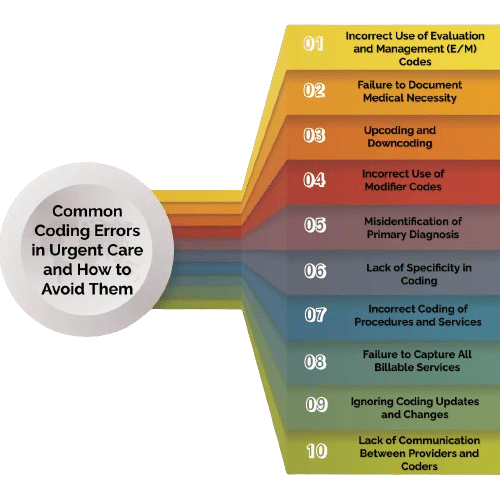
1. Incorrect Use of Evaluation and Management (E/M) Codes
Error: One of the most common coding errors in urgent care is the incorrect use of E/M codes. These codes are used to bill for patient visits and vary based on the complexity and time spent with the patient.
Solution: To avoid this error, ensure thorough documentation of the patient’s visit, including history, examination, and medical decision-making. Familiarize yourself with the specific criteria for each E/M level and use the appropriate code. Regular training and audits can help maintain accuracy.
2. Failure to Document Medical Necessity
Error: Medical necessity is a critical factor in determining the appropriate level of care and corresponding codes. Failing to adequately document medical necessity can result in claim denials.
Solution: Always document the reasons for the patient’s visit, the clinical findings, and the rationale for the treatments provided. This documentation supports the use of higher-level codes and ensures compliance with payer requirements. Training staff on the importance of documenting medical necessity is essential.
3. Upcoding and Downcoding
Error: Upcoding involves using codes that reflect a higher level of service than what was provided, while downcoding involves using codes for a lower level of service. Both practices can lead to compliance issues and financial losses.
Solution: Ensure that the codes used accurately reflect the services provided. Regular audits and cross-checks can help identify patterns of upcoding or downcoding. As an Urgent Care Medical Billing Expert Miami, FL, staying updated with coding guidelines and payer policies is crucial.
4. Incorrect Use of Modifier Codes
Error: Modifier codes are used to provide additional information about a service, such as when a procedure is modified or when multiple procedures are performed. Incorrect use of these codes can lead to claim rejections or incorrect reimbursements.
Solution: Understand the specific guidelines for using modifier codes. Use them only when appropriate and ensure they accurately reflect the circumstances of the service provided. Regular training and access to up-to-date coding resources can help avoid errors.
5. Misidentification of Primary Diagnosis
Error: Selecting an incorrect primary diagnosis can lead to claim denials or reduced reimbursements. This error often occurs when the diagnosis does not match the treatment provided or the reason for the visit.
Solution: Carefully review the patient’s medical records and ensure that the primary diagnosis accurately reflects the main reason for the visit. Cross-check the diagnosis with the treatments provided to ensure consistency. Continuous education and training in diagnostic coding are essential for accuracy.
6. Lack of Specificity in Coding
Error: Using nonspecific or generic codes can result in claim denials or reduced payments. Specificity is crucial in medical coding to accurately describe the patient’s condition and the services provided.
Solution: Use the most specific codes available to describe the patient’s condition and the treatments provided. Stay updated with the latest ICD-10 codes and guidelines to ensure specificity. Conduct regular coding reviews and audits to maintain high standards.
7. Incorrect Coding of Procedures and Services
Error: Errors in coding procedures and services, such as lab tests, imaging studies, and treatments, can lead to denied claims and compliance issues.
Solution: Ensure accurate documentation of all procedures and services provided. Cross-reference the documentation with the appropriate codes. Regular training and updates on coding guidelines are essential for maintaining accuracy.
8. Failure to Capture All Billable Services
Error: In the busy environment of an urgent care center, it is easy to overlook capturing all billable services, leading to lost revenue.
Solution: Implement a thorough review process to ensure all services provided are captured and coded correctly. Use checklists and electronic health records (EHR) to track services. Regularly review and update billing practices to ensure completeness.
9. Ignoring Coding Updates and Changes
Error: Coding guidelines and codes frequently change. Ignoring these updates can result in the use of outdated or incorrect codes.
Solution: Stay informed about the latest coding updates and changes from organizations like the American Medical Association (AMA) and the Centers for Medicare & Medicaid Services (CMS). Participate in ongoing education and training to keep up-to-date with the latest coding practices.
10. Lack of Communication Between Providers and Coders
Error: Poor communication between healthcare providers and coders can lead to misunderstandings and coding errors.
Solution: Foster clear and open communication between providers and coders. Regular meetings and training sessions can help ensure that both parties understand the importance of accurate documentation and coding. Encourage a team approach to coding and billing.
Tips for Accurate Coding in Urgent Care
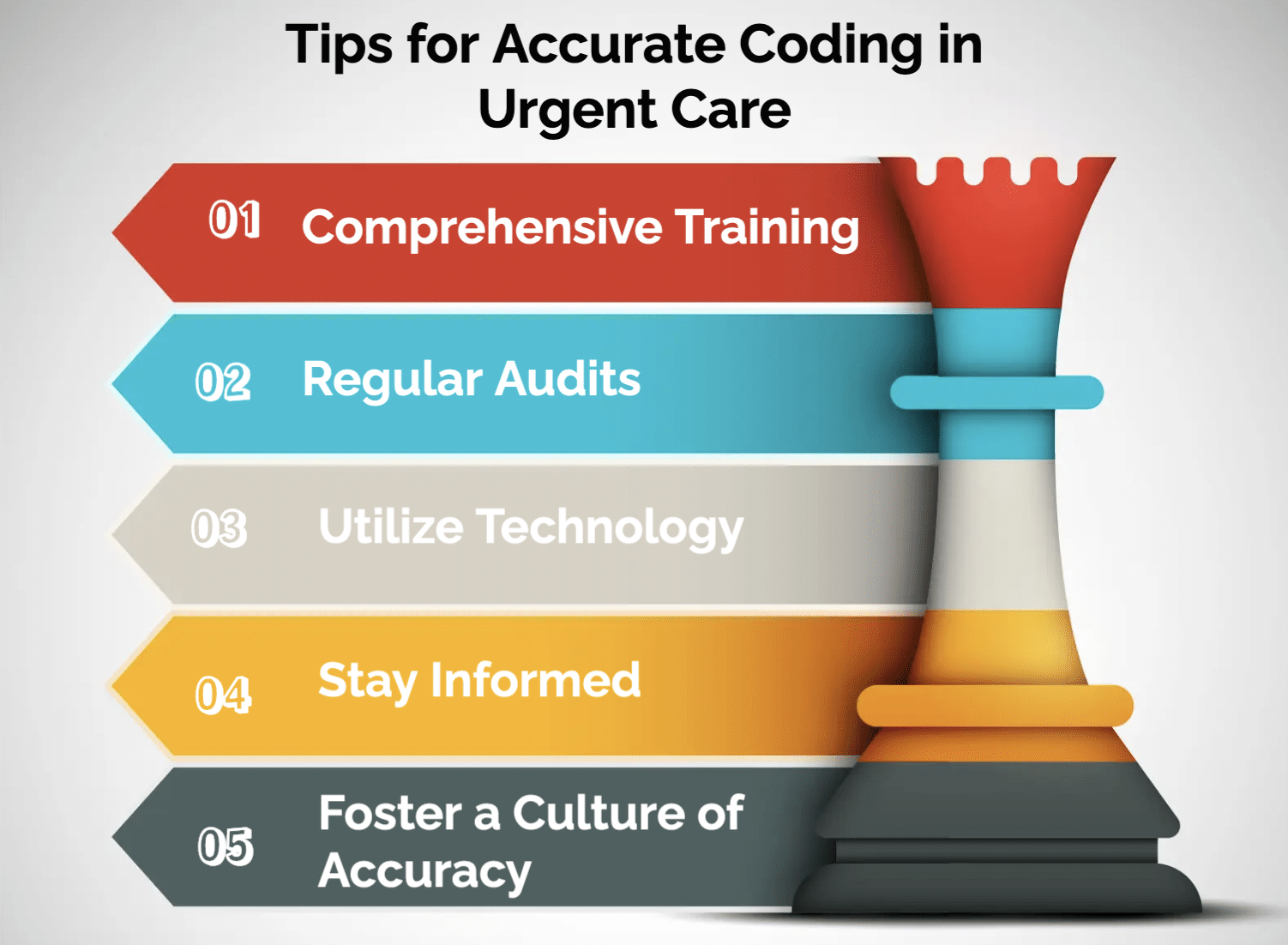
- Comprehensive Training: Invest in comprehensive training for all staff involved in coding and billing. Regularly update training programs to reflect the latest coding guidelines and best practices.
- Regular Audits: Conduct regular audits of coding and billing practices to identify and correct errors. Use audit findings to provide targeted training and improve processes.
- Utilize Technology: Leverage technology such as EHRs and coding software to streamline coding processes and reduce errors. Ensure that all staff are proficient in using these tools.
- Stay Informed: Keep abreast of changes in coding guidelines and payer policies. Subscribe to coding newsletters, attend workshops, and participate in professional organizations to stay informed.
- Foster a Culture of Accuracy: Encourage a culture of accuracy and accountability within the urgent care center. Recognize and reward staff for accurate coding practices and continuous improvement.
Conclusion
Accurate coding is crucial for the financial health and compliance of urgent care centers. By understanding common coding errors and implementing strategies to avoid them, urgent care facilities can improve their billing processes, reduce claim denials, and ensure appropriate reimbursements. As an Urgent Care Medical Billing Expert Miami, FL, your expertise in accurate coding and billing can make a significant difference in the success of urgent care operations. Prioritize continuous education, regular audits, and effective communication to maintain high standards of coding accuracy and efficiency.

