Mental health professionals face unique challenges when it comes to billing. Unlike many medical specialties that involve clear procedure codes and documentation rules, mental health billing is complicated by therapy session limits, prior authorization requirements, and varying coverage across insurance carriers. These complexities lead to frequent denials, delayed payments, and revenue losses that can burden providers. By outsourcing to expert medical billing services, practices can ensure cleaner claims, faster reimbursements, and more financial stability.
The Challenges of Mental Health Billing
Billing for mental health services is often more complex than for other specialties. Some of the most common challenges include:
- Frequent prior authorizations: Many insurance carriers require prior approval before patients can begin therapy or psychiatric treatment. Missing this step often leads to outright denials.
- Session limits and visit caps: Coverage for mental health often comes with limits on the number of therapy sessions allowed per year. Practices must track these closely.
- Varying coverage rules: Different insurers treat therapy, psychiatry, and telehealth visits differently, making claim submission inconsistent.
- Coding complexity: Incorrect use of CPT codes for therapy sessions, group counseling, or psychiatric evaluations is one of the top causes of denials.
- Documentation issues: Missing treatment notes, inadequate progress reports, or incomplete records often result in reimbursement delays.
Why are mental health claims denied so often?
Because of strict payer rules around session limits, authorizations, and detailed documentation, mental health claims are denied at higher rates than other medical specialties.
The Role of Mental Health Medical Billing Services
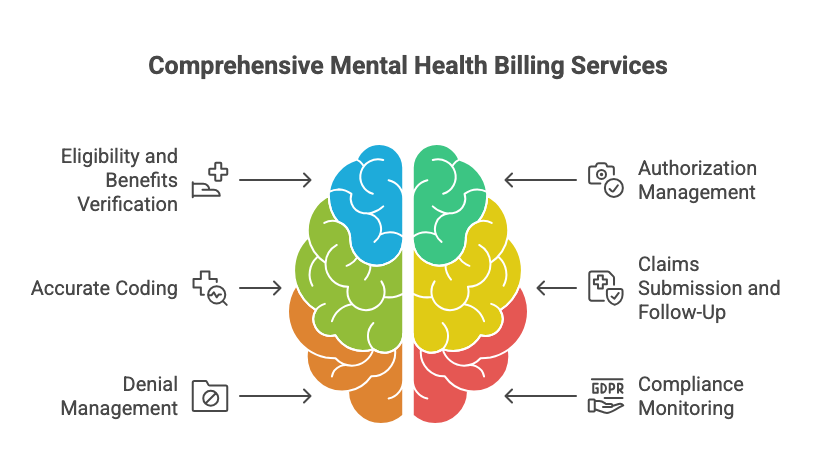
Professional mental health medical billing services are designed to address these unique challenges by combining deep knowledge of payer rules with advanced denial management strategies. These services typically include:
- Eligibility and benefits verification – confirming mental health coverage and session limits before treatment begins.
- Authorization management – securing pre-approvals for therapy, psychiatry, and intensive outpatient services.
- Accurate coding – ensuring CPT and ICD-10 codes for therapy, evaluations, and medication management are correct.
- Claims submission and follow-up – submitting clean claims and aggressively following up on unpaid or denied ones.
- Denial management – identifying denial trends and filing appeals with appropriate documentation.
- Compliance monitoring – staying updated with insurance regulations and HIPAA requirements.
By outsourcing these tasks, practices can reduce administrative burden and focus on delivering patient care instead of struggling with billing headaches.
Benefits of Outsourcing Mental Health Billing
The benefits of professional billing support extend far beyond faster payments. Mental health providers who use specialized services often experience:
- Reduced denials: Clean claims and proper documentation improve approval rates.
- Faster reimbursements: Streamlined processes shorten AR cycles and speed up payments.
- Higher revenue: Accurate coding and fewer errors reduce lost revenue.
- Lower administrative stress: Staff can focus on patient needs instead of payer disputes.
- Improved compliance: Billing teams ensure practices stay aligned with payer rules and HIPAA standards.
- Transparency in revenue cycle: Detailed reporting provides insights into payer trends and practice performance.
How do mental health billing services improve practice revenue?
By reducing denials, securing authorizations, and coding accurately, outsourced billing services help practices collect more of what they earn.
Specialty Scenarios in Mental Health Billing
Different types of mental health providers face unique billing challenges:
- Therapists and Counselors: Often struggle with session caps and ensuring proper documentation for continued therapy.
- Psychiatrists: Must bill for both evaluation/management and therapy codes, requiring precise coding to avoid denials.
- Substance Abuse Clinics: Face complex prior authorization processes and strict payer requirements for medical necessity documentation.
- Group Practices: Need to manage multiple providers under one NPI, which complicates claim submission and payment reconciliation.
- Telehealth Providers: Deal with modifiers, state-specific rules, and changing payer policies that affect reimbursement.
Expert mental health medical billing services adapt to each scenario, ensuring compliance and maximum revenue capture.
Best Practices for Mental Health Billing
Even with expert support, practices should follow these best practices to minimize issues:
- Verify insurance coverage and session limits before scheduling appointments.
- Obtain prior authorizations for evaluations, extended therapy, and intensive treatment.
- Use accurate CPT codes for all services, including group sessions and telehealth.
- Maintain thorough treatment notes and progress reports to support claims.
- Track denials by category to identify patterns and correct recurring errors.
- Regularly train staff on mental health billing updates and payer changes.
How can mental health practices avoid losing money on claims?
By combining strong documentation practices with outsourced mental health medical billing services, providers can significantly reduce denials and ensure timely payments.
FAQs About Mental Health Billing
What makes mental health billing more complex than other specialties?
Mental health billing involves session limits, prior authorization, and extensive documentation requirements that most other specialties don’t face.
Do all insurance companies cover therapy sessions the same way?
No. Coverage varies widely. Some carriers limit the number of sessions per year, while others require ongoing documentation to prove medical necessity.
Can outsourcing mental health billing save time for providers?
Yes. Outsourced mental health medical billing services allow providers to focus on patient care while billing experts manage claims, denials, and compliance.
Is telehealth covered under mental health billing?
Many insurers cover telehealth for mental health, but rules differ by state and payer. Correct modifiers and coding are essential for reimbursement.
How quickly can outsourcing improve cash flow?
Most practices see improvements within the first few months due to reduced denials and faster claim resolution.
Billing challenges shouldn’t prevent providers from delivering life-changing mental health care. With professional mental health medical billing services, therapists, psychiatrists, and clinics can simplify their revenue cycle, reduce denials, and ensure a steady cash flow.
Contact Gables Medical Billing today to learn how our team helps mental health practices recover lost revenue and stay focused on patient care.